You may have heard of the condition or seen a person in a delirious state portrayed in a movie or show – but what is Delirium? How is it caused and how is it diagnosed?
Here we discuss those FAQs and several others about Delirium. We also shed some light on the research being carried out at The Prince Charles Hospital (supported by The Common Good). It’s hoped that this research will help to make the condition easier to detect and prevent in the future.
Delirium: what is it?
Delirium is described as a serious disturbance in mental abilities that develops rapidly and severely impacts a person’s perception, cognition, and awareness.
As the brain is not functioning properly, the person who is delirious may struggle to interpret their surroundings or follow what’s going on. The symptoms can be terrifying and can cause significant distress for the patient and for family members who see them in a delirious state.
“They can hear and see things that aren’t real. They can feel things that aren’t real and when you put that all together it can be very much like you’re in a living nightmare,” said Associate Professor Dylan Flaws.
“In hospital, for example, you may not think you’re in hospital – you may think you’re in your bed at home, and you’re wondering why there are people in your room.”
A/Prof. Flaws says those who experience the condition can jump to frightening conclusions, for example thinking those trying to help them and care for them in hospital are burglars or worse.
“You can worry about what’s in the drip that’s attached to your arm. You are worried, ‘Are they poisoning me?’ things like that,” A/Prof. Flaws said.
And as their brain is not functioning properly and they cannot comprehend the situation, their distress continues or can escalate.
Symptoms of Delirium
Delirium is an organic cerebral condition (a condition which involves the brain’s function decreasing over a time period) with psychiatric symptoms.
These symptoms will depend on the type of Delirium (hyperactive, hypoactive or mixed) being experienced, but may include:
- Cognitive impairment such as memory loss, disorientation, difficulty communicating
- Behavioural changes such as agitation, aggression, restlessness, hallucinations, lethargy
- Reduced Environmental Awareness
- Emotional Disturbances such as depression, mood swings, fear, irritability
Hyperactive Delirium vs Hypoactive Delirium
A person with Hyperactive Delirium may appear hyper alert, anxious, restless, agitated and aggressive. They may also experience delusions or hallucinations.
On the other hand, a person with Hypoactive Delirium may appear drowsy, reserved, withdrawn, lethargic and distant.
“That’s the insidious group who often have a worse outcome because it takes even longer for it to be recognised” said A/Prof. Flaws.
“Often with a Hypoactive Delirium, they’re lying in the bed, they haven’t pushed their buzzer. The nurse will come up to clear their lunch and they’ll see the breakfast tray and the lunch tray right next to each other and not a single piece of food has been touched and the patient is just looking at the ceiling. And they look calm but when they try to get their attention it’s very hard to get their attention, and then you say, ‘Do you know where you are?’ and they say, ‘No.’”
People can also have Mixed Delirium and exhibit qualities of both Hyperactive and Hypoactive Delirium.
Dementia vs Delirium
Symptoms of Dementia and Delirium may appear similar and a person with Dementia may experience Delirium.
Simply put, dementia is a permanent, chronic, gradual decrease in brain function that happens over a longer period. It also and progresses more year after year. Whereas delirium is temporary and can happen very quickly – overnight or within a matter of hours.
“That’s how you can tell this is not the climate, this is the weather. This is a thunderstorm that’s going on in their brain and we need to work out what’s causing it,” said A/Prof. Flaws.
What causes Delirium?
Delirium may be triggered by one or multiple stressors placed on the brain.
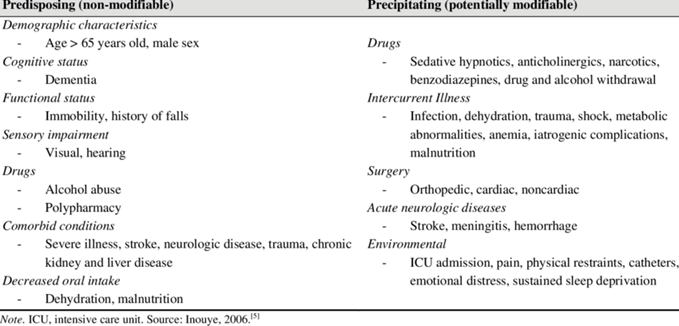
Those stressors can include predisposing factors like dementia or age, or precipitating factors like an acute illness or infection. It can also be triggered when a new medication is started.
“The more of those that you have at any one time, the more the brain has to deal with and at a certain point it gets overwhelmed,” said A/Prof. Flaws.
“The delirium is the smoke – it’s the thing that tells you something is on fire.”
Who is at risk of Delirium?
Anybody can experience delirium, but there are a range of predisposing risk factors including age and cognitive impairment.
“If you’ve got fresh tarmac, a beautiful road that you’ve paved, and there’s a thunderstorm, you’re going to drive a bit slower to get to work but you’re going to get to work. But if you’ve got a road that’s been there for 65 years, and you get that same thunderstorm the bridge might wash out and you may not get to work. That’s why they’re predisposed. Their brain is more vulnerable to those insults. It’s less resilient to withstand them.” said A/Prof. Flaws.
How is Delirium diagnosed?
Delirium is usually diagnosed by an experienced clinician. Patients are accessed according to the description of Delirium in 5th edition of the Diagnostic Statistical Manual for Mental Disorders (DSM 5).
Unfortunately, the condition is a challenge to diagnose. In fact, it is frequently misdiagnosed as it can present like a range of other conditions such as psychosis or depression.
Yet it is known that the longer a person is in a delirious state the bigger the impact it has on their cognitive function. That’s why further research into this area is needed.
“If you don’t have the right diagnosis, you don’t get the right treatment,” said A/Prof. Flaws
“And the problem is, with most of the things that we treat – if you treat psychosis or depression – you’re giving them another medication and that medication is another thing the brain has to deal with.”
To help clinicians, a range of screening tools are available to be used in different settings that help staff flag who might be delirious.
How is Delirium treated?
To treat delirium, it is a case of medical professionals working out why a person has become delirious and addressing that underlying cause.
“There is no scan that picks up delirium, there is no blood test, and there’s no magic pill that makes it go away,” said A/Prof. Flaws.
If there is an infection, this is treated. Medication regimes are reviewed and simplified where possible.
A/Prof Flaws says the best thing to do is to prevent delirium from occurring in the first place.
“Look for the things that could cause delirium, look at who is at risk of developing delirium and then making sure that we do everything in our power to prevent them developing a delirium.”
This can include promoting good sleep and nutrition, getting patients out of bed and mobilising, and keeping them socially and cognitively engaged and grounded.
What happens if it is not treated?
It is important to treat delirium as early as possible. It is described as a “toxic state” for the brain to be in.
“It’s like having sand in your motor. The longer it’s in there the more damage it’s doing,” said A/Prof. Flaws.
“The longer a person is delirious for, the bigger the impact it has on their cognitive function afterwards.”
A person can be in a delirious state until the cause is treated.
A/Prof Flaws says if delirium gets better and it hasn’t been detected or addressed, then the person is very lucky.
If it hasn’t been detected, the outcome can be disastrous.
“If it gets worse, the person can die of sepsis, they can have a fall, they can sustain further injuries,” said A/Prof Flaws.
Research into Delirium at The Prince Charles Hospital
The primary focus of research being carried out at The Prince Charles Hospital and supported by The Common Good is the prevention of delirium.
“We need to do better at picking this up, treating it, and preventing it,” said A/Prof Flaws.
“It’s been shown that a delirium prolongs the length of stay, increases the risk of admission and increases the risk of death – all of which you want to prevent.”
So far, research has been carried out looking at the risk factors for delirium.
An electronic screening tool called EDIS-ICU is being validated in Estonia, Japan and Australia at present. This is a language free, culturally neutral app that staff can use on any digital device to screen for delirium at the bedside. This study is ongoing, but those involved are assessing if the app can help to detect delirium and if it does it, is early enough.
The ICU of the Future project also aims to reduce cases of ICU delirium by improving the ICU environment to promote quality sleep and rest, as well as cognitive engagement and hopefully improve patient outcomes.









